Unlocking Insights | The Power of Behavioral Health Outcome Measurement in Your Organization
By measuring behavioral health outcomes, you can gain crucial insights to impact all areas of your organization. You can monitor patient progress, assess the effectiveness of interventions and treatments, and identify areas for potential improvements. Armed with better outcome measurements, you can improve communications between providers, patients, caregivers, and families. You can also build stronger relationships with insurers, who are increasingly focused on data-driven approaches to behavioral health such as value-based care (VBC) models.
This is an exciting time for behavioral health organizations that want to adopt a more data-driven approach. The digital health solutions many organizations have adopted to expand patient access and streamline operations can also fuel a robust outcome measurement program. Whether monitoring scheduled and billed appointments, assessing resource usage patterns, or tracking program completion rates, digital solutions can help you collect, analyze, and share outcome measurements that transform data into powerful insights.
Let’s consider how technology, such as electronic health record (EHR) systems, telehealth software, and a strong patient portal can help improve outcomes for patients, payers, and your organization. We’ll look at:
- Data automation to fuel greater organizational efficiency
- Patient outcomes and patient engagement
- Insurer expectations for outcomes measurement
- How digital tools can help your organization thrive
Streamlining operations by automating data collection and management
Integrated digital behavioral health solutions make it possible to automate the secure collection, analysis, and management of data. This is an important step in building a data-driven approach to behavioral health, as it enables more efficient and accurate tracking of patient outcomes. Instead of providers or administrators having to manually aggregate data from disparate platforms or paper, you can focus on gleaning insights from across your operations in a standardized way. By automating the collection of data, you can also free up over 14% of provider and administrator time. This means that providers spend more time providing care and less time on manual work, saving them and your organization time and money. The image below highlights to ROI (return on investment) your organization can achieve by investing in an integrated patient portal and EHR platform that automatically tracks patient outcomes.
Optimizing patient engagement and experience across the continuum of care
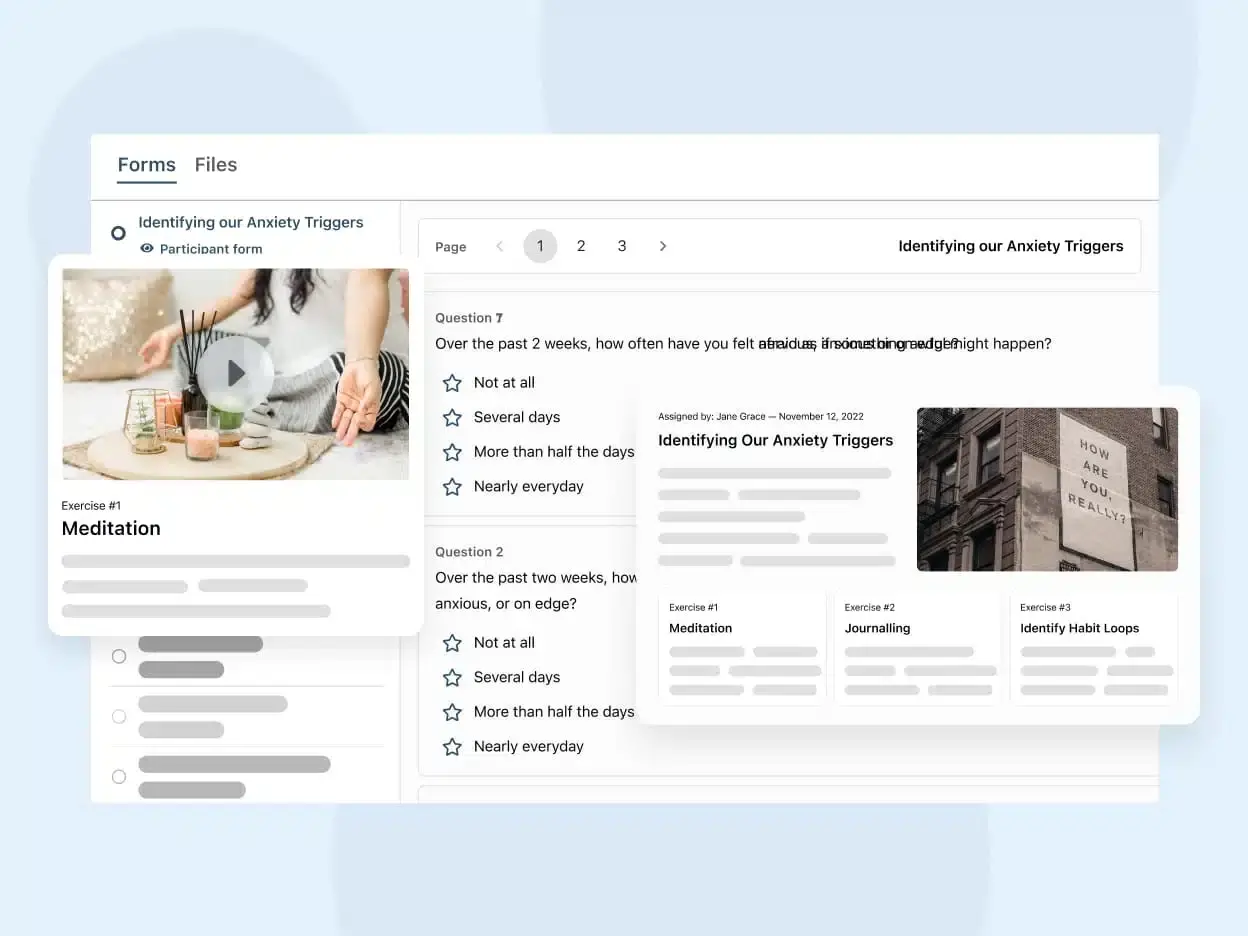
Telehealth and a patient portal make it convenient for patients to engage with providers and support staff when onsite care isn’t an option or isn’t preferred by the patient. They can self-report through online forms from a mobile or desktop app, increasing both the likelihood of treatment compliance and the frequency of data collection. These same tools can provide patients with additional care options to support learning and skills development outside of scheduled sessions with providers, such as digital learning modules and online instant messaging access. For providers, integrating your EHR, telehealth platform, and patient portal makes it easier to monitor patient symptoms, tailor ongoing support, and assess progress over time.
All of this has the added benefit of giving you more client- and program-specific data across the continuum of care and your operations. You can see beyond the silos that often exist to determine what’s working well and what might need improvement to ensure the best engagement and experience.
Improving insurer relationships and funding
For payers, data speaks volumes. Digital behavioral health solutions lay the foundation for building more positive insurer relationships and funding sources on the strength of your outcome measurements. With telehealth software, for example, you can deliver comprehensive programs with reimbursable services that address patient needs through their care journey. Then, you can set performance metrics and use real-time analytics to optimize programs and clearly demonstrate the value provided. Armed with data-based outcome measures, you can make decisions about what areas of your organization need more resources, which process should be optimized, and which services can be scaled for growth. You can also influence reimbursement negotiations and explore more data-driven business models that are attractive to insurers.
How Telehealth can Help
Build a better outcome measurement program with Qualifacts’ OnCall Health patient portal
In a data-driven world, savvy behavioral health organizations need scalable, streamlined ways to leverage data to improve outcomes. Qualifacts’ patient portal, OnCall Health, gives you the tools you need to build an integrated outcome measurement program that streamlines operations for your organization, improves the patient engagement experience, and reframes relationships with insurers based on evidence of performance.
Learn more how Qualifacts’ OnCall Health can help you turn outcome measurement into a strategic advantage for your organization by booking a call with our expert team.