Why Is Denial Management Critical for Reducing Healthcare Revenue Loss?
By some estimates, nearly a third of healthcare entities lose about 10% of their revenue from denied claims, adding up to billions of claim dollars every year that may never see reimbursement. Experts estimate that providers could avoid 86% of denials, so it’s not surprising that most providers (three out of four) are prioritizing better denial management.
As alarming as this trend is in healthcare overall, behavioral health organizations grapple with uniquely complex challenges, including:
- Complex diagnoses and treatment procedures that can lead to coding errors.
- Complex insurance requirements and the lack of standardized denial rules for behavioral health.
- The resource-intensive process to support appeals with detailed narratives and case note documentation.
- The legacy of manual, paper-based processes.
- Increasing prevalence of alternative payment models such as value-based care.
In this article, we’ll consider strategies that revenue cycle leaders in behavioral health can use to reverse this trend with a proactive denial management approach.
Estimating Revenue Loss from Denied Claims
To start, it can be eye-opening to estimate your revenue loss from denials. If you’re not already tracking this number, here’s a simple formula: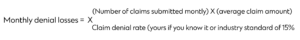 Also consider how much you could recover. Here’s another simple formula to estimate your potential recovery opportunity, assuming an industry average rate for denial recovery of 67%:
Also consider how much you could recover. Here’s another simple formula to estimate your potential recovery opportunity, assuming an industry average rate for denial recovery of 67%:
Potential denial recovery = Revenue loss from denials X 67%
To illustrate how this works, here’s a simple scenario. If your practice submits 2500 claims every month that average $200 each and your claim denial rate is 15%, you risk losing $75,000 every month. The good news is that managing denials could help you recoup an estimated $50,250.
Building a Proactive Denial Management Program
While achieving zero denials may be impossible, addressing preventable issues can simplify appealing denials and recouping revenue. By analyzing historical denials data, identifying root causes, and implementing corrective measures across front-office and backoffice teams, you can adopt a more assertive approach that significantly improves productivity, impacts cash flow, and contributes to a better patient experience. Let’s look at six different strategies you can adopt now to transform your denial management practice.
Validate Referrals and Authorizations
Invalid referrals and prior authorizations account for about 18% of denials. Many behavioral health services, such specialized treatments or those for severe mental illnesses, may require prior authorizations. Improving front-end revenue cycle management is essential to prevent denials from occurring and becoming an issue to manage later on.
Leverage capabilities in your EHR platform to streamline patient registration, insurance verification, and pre-authorization. Build double-checking of referrals and authorizations into processes to make sure that all required permissions are obtained up front; this is critical for treatments or modalities that may not be understood or are new in behavioral health. By identifying potential problems early on, such as lapsed coverage or incorrect patient information, you can make sure that potential billing issues are addressed before services are provided or claims are submitted. This can also help you swiftly rework denied claims.
Automate Claims Processing
Submitting a clean claim the first time, and on time, is by far the best way to reduce denial rates. Automating claims submission can lead to leaner claims by reducing human errors, improving data accuracy, and streamlining the entire billing process. In fact, automation can reduce the cost of the claims journey by as much as 30%, increasing the first-time pass rate and reducing the risk of denials. Using technology that is integrated into existing systems, such as Qualifacts EHRs and our revenue cycle products and services, can make it easy for staff, practitioners, and clients to access and use. This in turn helps create a smooth claims process that reduces the volume of denials you have to manage.
Automate Denial Management
Many organizations still rely on manual processes to manage denials, even though it can be complex and labor-intensive. As a result, many denials go unchallenged because organizations lack the resources to follow up. Just as with claims processing, you can use technology to efficiently manage denial management without adding staff. Automating denial management workflows can help you:
- Assess the business impact of each denial and prioritize denials that have the best opportunity for quick revenue recovery.
- Manage bulk appeals where claims to process claims with the same payer and cause of denial.
- Process and route denial follow-up tasks to appropriate billing staff.
- Coordinate communication between payers, clients, and internal staff.
- Group complex claim denials and route for review by a senior billing professional.
- Ensure appeal deadlines are met.
- Improve denial resolution speed.
Monitor Analytics
Behavioral health care services come with unique billing codes and specific claims requirements.These services can be misunderstood or incorrectly coded. Denial management is a data-driven approach. Implementing analytics tools that integrate with an EHR platform can give you valuable insights into recurring issues, payer-specific challenges, misunderstandings or misinterpretations related to specialized treatments or therapies, and other common billing issues.
Reviewing denial analytics should be a regular task, helping you pinpoint reasons that recur or that are trending. Armed with this information, you can:
- Pinpoint denial trends and devise targeted strategies to address root causes.
- Negotiate with payers based on data.
- Gain insights about billing issues that are happening in front-end and middle-stage revenue cycle teams.
- Analyze workflow performance and track staff productivity related to denied claims to better understand the impact to your business.
Stay Current
Behavioral health trends, such as the rise of telehealth during the pandemic or medication-assisted treatment (MAT) programs, can change rapidly and may influence how services are understood and billed by payers. So that your staff is always prepared to address new billing complexities, it’s vital to keep everyone up-to-date with trends as they develop and adapt billing processes to accommodate new services and requirements successfully.
Partner with a behavioral health revenue cycle management service
Outsourcing revenue cycle management can be an efficient way to get the resources and expertise you need to tackle denials, whether you’re clearing a denial backlog or implementing a robust denial management program. A partner such as Qualifacts, with deep experience in behavioral health care billing, can provide systems and processes to analyze denials, identify and interpret patterns and trends, track appeals, and provide insights that ensure consistent cash flow, so your team can focus on core business.
For behavioral health organizations, the skyrocketing rate of denied healthcare claims warrants urgent revaluation of all billing processes and strategies. Adopting a proactive denial management approach should be part of a comprehensive revenue cycle management strategy. By automating and streamlining processes and adopting best practices to track denial trends, behavioral health organizations gain a powerful tool to ensure they maximize the claims revenue they deserve.
